Empathy? Sympathy? Compassion: More Than Just a Feeling in Healthcare
The concept of empathy has been swirling around in my head ever since a quiet afternoon at my parents’ house, where a simple ad on TV caught my attention. Believe it or not, TV still exists—yes, even with ads! It was part of a campaign by the Health Promotion Board (HPB), urging people to offer support with empathy when someone reaches out to them.
That brief, yet powerful message got me thinking: What is empathy, and how does it really differ from sympathy or even compassion? We often use these terms interchangeably in healthcare and even try to teach empathy to our juniors, but they carry distinct meanings. When healthcare providers can truly connect with patients on an emotional level, it not only builds trust but also improves patient outcomes. But here’s the big question: Can empathy be too much of a good thing? And is it always necessary?
Empathy vs Sympathy
The term empathy originates from the German word “Einfühlung,” which was coined in the late 1800s and roughly translates to “feeling into.” Not all researchers agree on the definition of empathy - psychologist Judith Hall called it “ a fundamentally squishy term.” So what exactly is empathy, and how does it differ from sympathy?
As Brené Brown famously puts it: “Empathy fuels connection. Sympathy drives disconnection.” In her video, Brown explains that empathy is about truly connecting with someone by feeling with them. It means entering their emotional world and acknowledging their feelings without trying to fix them or offer advice. In contrast, sympathy is more about feeling for someone but from a distance. It's like looking down into someone’s dark hole and saying, “That looks rough,” without actually climbing in. Brown breaks empathy down into four key components:
Perspective-taking – the ability to put yourself in someone else’s shoes.
Staying out of judgment – just listening, without offering critique or advice.
Recognizing emotions in others – understanding feelings you may have experienced yourself.
Communicating that recognition – letting the person know you see and understand what they’re feeling.
In healthcare, this distinction becomes even more critical. Empathy fosters genuine connections that make patients feel heard, while sympathy can sometimes come across as detached or dismissive. Understanding the difference between these two is key to providing compassionate care.
The Power of Empathy in Medicine—and Its Limits
Empathy can be transformative in healthcare. Studies have shown that when patients feel emotionally understood, they are more likely to trust their doctors, follow treatment plans, and experience better health outcomes. But empathy doesn’t come without a cost.
Empathy, especially in high-stress medical environments, can lead to what’s known as empathic distress. This is a form of emotional burnout where the constant exposure to others' suffering wears down the healthcare provider, making it harder to maintain their own emotional well-being. While empathy is essential for good care, an overload of emotional involvement can leave doctors and nurses feeling drained, anxious, and even less effective in their roles.
Can Empathy Be Taught, or Is It Innate?
So, can empathy be taught? It’s a hot topic in medical education. Many schools are introducing courses focused on building emotional intelligence and narrative medicine, with the goal of fostering empathy. Through role-playing, reflective listening, and patient storytelling, students learn to develop empathy as a skill.
Yet, some argue that while empathetic behaviors—such as active listening, maintaining eye contact, and expressing concern—can be learned, true emotional empathy might be something you’re born with. There’s an ongoing debate about whether empathy is a natural trait or something we can cultivate over time.
Faking Empathy: Does It Really Matter?
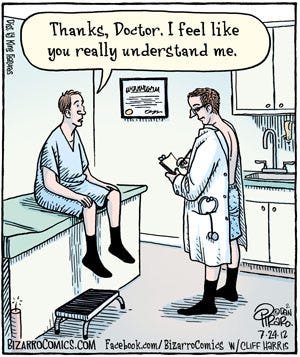
Here’s another layer to the debate: Can empathy ever be “faked”? Some skeptics suggest that healthcare providers may learn to simulate empathy without genuinely feeling it. They might adopt the right behaviors—asking thoughtful questions, nodding appropriately or expressing concern—without the emotional connection that defines true empathy.
Source: https://memeguy.com/photo/454857/-empathy
But does it really matter if empathy is genuine? I don’t know and the answer may never be found (I would be seriously amazed if healthcare professionals admitted to faking empathy even when they weren’t feeling very generous- but then again, I remained to be surprised as there was a paper of doctors admitting that they picked their noses!)
So I turned to my own family and asked them if it mattered if their doctor was faking it? My dear old dad, in his typical Swedish manner, told me, “Vicky, we used to call it $#@@ing BEDSIDE MANNERS! It doesn’t matter if he’s faking it! Stop with these new-age terms.” Maybe he’s right. As long as healthcare providers display empathy convincingly, patients are likely to feel heard and supported. And for some, the benefits of “faked” empathy might be just as valuable as the real thing.
Striking a Balance: Empathy, Compassion, and Emotional Well-Being
While empathy is about feeling and understanding another person’s emotions, compassion takes things a step further—it’s about turning that emotional connection into meaningful action. Compassion is often described as the desire to alleviate suffering. Where empathy allows you to feel what someone else is going through, compassion drives you to do something about it. In healthcare, the key to sustainable empathy may lie in finding a balance between emotional connection and professional distance. Too much empathy can lead to burnout, while too little can leave patients feeling disconnected. This is where compassion offers a crucial middle ground, allowing healthcare providers to take action and provide care without becoming emotionally overwhelmed.
Derived from the Latin word meaning "to suffer with," compassion, like empathy, is complex and multifaceted, with varied definitions in the literature. For example, a doctor working in a high-stress environment like an ICU may empathize with their patients’ suffering but must also maintain emotional distance to avoid burnout. Instead of absorbing all the emotional weight, the doctor can focus on what they can do—whether it’s ensuring the patient is comfortable, offering support, or finding ways to communicate with their family. In this way, compassionate actions become the driving force behind effective care, enabling providers to offer meaningful help without becoming overwhelmed.
Conclusion: Empathy in Motion
The key difference between empathy and compassion lies in this active response. Empathy can be overwhelming, especially when healthcare providers are deeply in tune with their patients' suffering. Compassion, on the other hand, allows for emotional engagement while maintaining enough distance to protect the provider’s well-being. It provides a path for healthcare professionals to respond effectively without being emotionally drained, ensuring that the focus remains on relieving the patient’s distress.
Further Resources
Empathy, sympathy and compassion in healthcare: Is there a problem? Is there a difference? Does it matter? Excellent paper which discusses in clearly greater and much more scholarly detail than this substack ever will reach
What is Empathy? A lovely BBC Crowdscience episode that started with a listener’s question -Maria gets a headache when her husband gets migraines. She wants to know if she's experiencing an extreme form of empathy and what’s happening in her brain to cause this.
Victoria Ekstrom is a narrative medicine advocate who’s constantly seeking the balance between compassion and professional distance. Unafraid to risk a scolding from her father in pursuit of “journalistic truth”, she’s committed to exploring the deeper human side of healthcare. When she’s not writing or pondering empathy’s role in medicine, she’s chasing after her two kids, her dachshund, and—occasionally—new inspirations from unexpected places (like TV ads).